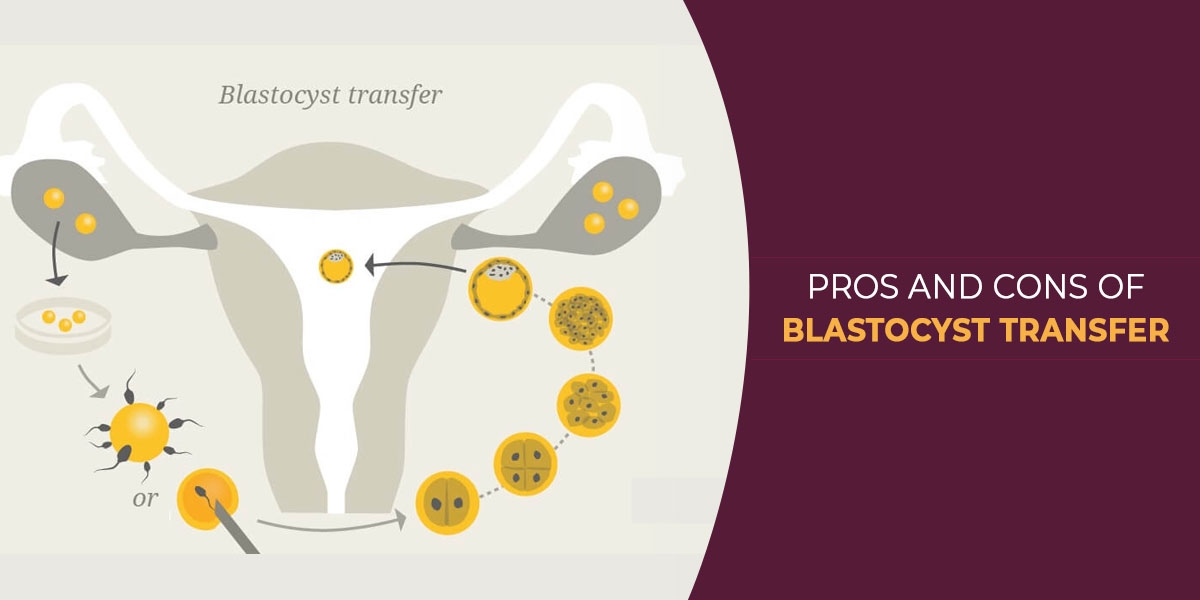
Blastocyst transfer is a method in which the embryo is allowed to develop into a blastocyst before it is transferred to the mother’s uterus. This technique has shown unique results and has been very successful. The blastocyst transfer is presently being used more often for the IVF treatment.
Pros of Blastocyst Transfer
The blastocyst transfer permits the embryologist to pick the best quality embryo for the IVF procedure. The quality of the embryo is very imperative to establish the success of the pregnancy. Some embryos do not become blastocysts; therefore apt monitoring of the embryo development and growth over the 5 to 6 day period is required. This is to ensure that the embryo selected for the IVF procedure is healthy and has a strong survival chance. In the blastocyst transfer, minimum embryos are transferred to the uterus and this decreases the chances of multiple pregnancies. Patients frequently ask for multiple embryos to be transferred to the uterus in the hope of increasing the probability of a successful gravidity. With the blastocyst transfer the positive outcome rate is much higher hence usually only one or two blastocysts are transferred to the uterus. 25% of the times when two embryos are transferred they both implant. In a natural pregnancy the egg is fertilized in the fallopian tubes in which it takes over 3 days for the embryo to reach the uterus where it hatches and begins implantation by the 6th day. The blastocyst transfer adheres to the sequence of the natural process quite closely. By transferring the egg when it is 5 or 6 days old the uterus is ready for it and the embryo almost immediately starts attaching itself to the uterus wall.
The Blastocyst starts to hatch in the lab prior to it transferred to the uterus. Hatching is a necessary stage in the success of the IVF procedure. Failure of the embryo to start hatching by the 6th day a technique called assisted hatching can be used. Furthermore, blastocyst transfer allows the doctors to monitor and assist in the hatching if required. This improves the chances of getting pregnant, which is a very great advantage of the blastocyst transfer and has assisted to really improve the success of the IVF procedure. Some embryos arrest before the 5th day. Many times in the 2-3 day transfer, it was found the embryo has arrested and the IVF procedure failed due to this. The blastocyst transfer helps to do away with the possibility of transferring embryos that will die off before day 5 and ensures a higher embryo survival rate. Elimination of abnormal embryos is easy during the development of blastocyst. In which embryos with chromosomal abnormalities usually do not reach the blastocyst stage and they are also arrest before the 5th day. Pre-implantation genetic screening (PGS) process is very easy on a blastocyst, as more cells are available for extraction and testing. This test helps to remove abnormal embryos and guarantee a good embryo without any genetic defects is passed during the IVF procedure. Usually an embryo with a defect undergoes cessation after a while. In cases where abnormal embryos have been transferred in the 2-3 transfer procedure, even if these embryos do implant, it resulted to a miscarriage. Conclusively, the Blastocyst transfer reduces the rate of early miscarriages as well. Approximately 40% of the embryos do not become blastocysts, these could be abnormal embryos or defective embryos or just weak embryos which have a low likelihood of survival. The blastocyst transfer has enabled couples to have healthier babies with less birth defects and abnormalities.
Cons of Blastocyst Transfer
Suboptimal condition of the culture environment will lead to delayed embryo development and even embryonic arrest at least in some cases. Furthermore, if the culture system and quality control in an IVF lab are epileptic in nature, good results will not be obtained with extended culture to day-5. Such procedures will do better with day-3 embryo transfers – putting back the embryos earlier, before they are “stressed” too much in the weak culture environment. Also in patients with low number of good quality embryos (2-3), there is no added advantage of embryo selection, so there is no benefit of culturing in the lab for 2 additional days with the added risk that there might be no good embryo left for transfer, in such cases it is better to transfer earlier itself.